这次总统大选,让很多美国人都在思考两党还有没有可能合作。
如果从数百万身患癌症和其他疾病的患者角度考虑,我希望仍然有合作的可能。因为18年前,我罹患致命的非霍奇金淋巴瘤(NHL)时,两党合作帮我捡回了一条命。
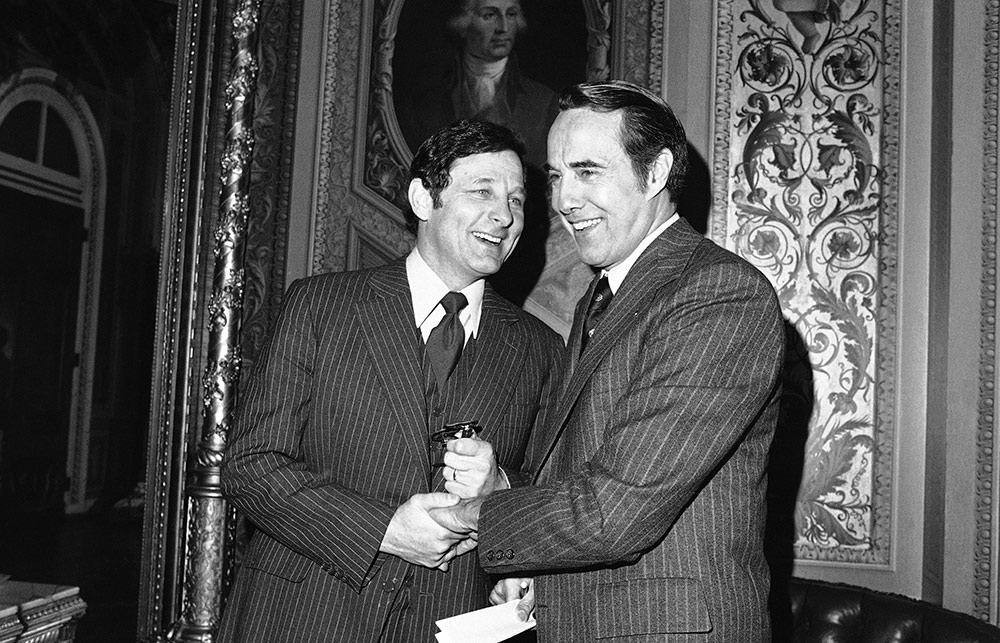
拯救我的药物来自多年研究,但如果不是印第安纳州民主党人伯奇•拜赫和堪萨斯州共和党人鲍勃•杜尔两位参议员在1980年提出法律,研究成果就无法帮到我。
该项法律被称为《拜杜法》(Bayh-Dole Act),允许大学、小企业和非营利组织拥有联邦资助的早期发明专利权。相关机构可以将知识产权授权给有资源和经验的私营公司,将有应用前景的创意转化为能够普遍使用的药品。与私营部门合作很有意义,因为大学实验室通常缺乏资源和人力,无力支持漫长昂贵的研究、测试和研发过程从而孵化创意。
在《拜杜法》之前,知识产权所有权均由政府掌握,偶尔转化为实际产品向病人提供。当该法通过时,政府掌握发明中只有不到5%获得商业生产许可。政府控制专利权期间,没有一种药物由联邦政府支持的研发部门研发。
不过,幸运的是,参议员拜赫和杜尔暂时搁置党派偏见,成功打破了僵局。具有里程碑意义的法律为私营公司搭建法律框架,后来推动200多项突破性的医疗创新,拯救我的创新就囊括其中。
2002年1月,我被诊断出非霍奇金淋巴瘤,是不治之症,当时唯一的治疗选择就是化疗。众所周知,化疗能够减缓病程,但最终不可避免复发。当时,确诊到死亡的平均寿命只有8年。得知无法跟丈夫一同老去,也看不到孙子孙女读完小学,我心里非常难过。
然而化疗并未减缓病情发展。治疗了几个月,该病的新疗法及时上市,即放射免疫疗法(RIT)。新疗法跟化疗不一样,化疗同时攻击癌细胞和健康细胞,治疗多达8次,RIT只针对癌细胞,而且只需注射一两次。
2002年9月,我注射了两剂最先进的RIT药物替伊莫单抗,之后病情逐渐减轻,身体基本健康。如果不是医疗创新,我的生活可能遭遇非常不一样的转折。
替伊莫单抗治疗方案中的关键部分是注入利妥昔单抗,该药可以减少血液中癌性B细胞数量。斯坦福大学(Stanford University)的研究人员利用美国国家卫生研究院(National Institutes of Health)的资助,在20世纪70年代和80年代发现该种B细胞技术。
但将想法变成切实可行的治疗方法需要大量时间和投资。如果不是当初研究人员离开斯坦福大学并于1985年成立Biotherapy Systems,进一步开发和商业化B细胞技术,医学发现可能永远没有机会变成在商业上可行的癌症疗法。
仅仅一年后,Biotherapy Systems与IDEC制药公司合并,成功实现了B细胞疗法。产品经过多年调整,IDEC于1993年开始利妥昔单抗临床试验。到1995年,生物技术巨头基因泰克(Genentech)与IDEC联手实施微调。
1997年,美国食品与药品管理局(FDA)终于批准,将利妥昔单抗的商标定为美罗华。
多亏1980年法律允许技术转让,否则该研究可能在斯坦福实验室就已经夭折。正因为《拜杜法》的推动,私营部门才成功开创了市场化药品。
我并不是唯一靠《拜杜法》支持的药物创新系统救回一命的病人。根据该法律,私营公司能够为病人提供数百种治疗方法,包括癫痫药物普瑞巴林、卵巢癌和乳腺癌药物紫杉醇,以及多发性硬化药物Tcelna等。
不过,目前社会活动团体正在向政客施压,要求利用法律中从未使用过的条款夺取新冠药物的专利权,这对私营制药公司和患者都不是好消息。该做法并无法律依据,因为《拜杜法》只允许政府在极少数情况下获得专利,比如当某家公司未广泛提供产品时。尽管面临各种压力,立法者仍需合作,维持《拜杜法》的保护力度。
因为事关人命。
患者应该感谢参议员拜赫和杜尔,因为两人认识到授权私营制药公司将政府资助的研究转化为药物和疗法无关党派。后来提案在国会通过,当时罗纳德•里根刚刚赢得大选,而吉米•卡特仍然在任。当年两党愿意携手推动公共卫生,帮助跟我一样与病魔抗争的人,现在这种精神应该延续。(财富中文网)
贝齐•德帕里是病人利益代言人,也是《癌症之地历险记》(Adventures in Cancer Land)一书作者。
译者:冯丰
审校:夏林
这次总统大选,让很多美国人都在思考两党还有没有可能合作。
如果从数百万身患癌症和其他疾病的患者角度考虑,我希望仍然有合作的可能。因为18年前,我罹患致命的非霍奇金淋巴瘤(NHL)时,两党合作帮我捡回了一条命。
拯救我的药物来自多年研究,但如果不是印第安纳州民主党人伯奇•拜赫和堪萨斯州共和党人鲍勃•杜尔两位参议员在1980年提出法律,研究成果就无法帮到我。
该项法律被称为《拜杜法》(Bayh-Dole Act),允许大学、小企业和非营利组织拥有联邦资助的早期发明专利权。相关机构可以将知识产权授权给有资源和经验的私营公司,将有应用前景的创意转化为能够普遍使用的药品。与私营部门合作很有意义,因为大学实验室通常缺乏资源和人力,无力支持漫长昂贵的研究、测试和研发过程从而孵化创意。
在《拜杜法》之前,知识产权所有权均由政府掌握,偶尔转化为实际产品向病人提供。当该法通过时,政府掌握发明中只有不到5%获得商业生产许可。政府控制专利权期间,没有一种药物由联邦政府支持的研发部门研发。
不过,幸运的是,参议员拜赫和杜尔暂时搁置党派偏见,成功打破了僵局。具有里程碑意义的法律为私营公司搭建法律框架,后来推动200多项突破性的医疗创新,拯救我的创新就囊括其中。
2002年1月,我被诊断出非霍奇金淋巴瘤,是不治之症,当时唯一的治疗选择就是化疗。众所周知,化疗能够减缓病程,但最终不可避免复发。当时,确诊到死亡的平均寿命只有8年。得知无法跟丈夫一同老去,也看不到孙子孙女读完小学,我心里非常难过。
然而化疗并未减缓病情发展。治疗了几个月,该病的新疗法及时上市,即放射免疫疗法(RIT)。新疗法跟化疗不一样,化疗同时攻击癌细胞和健康细胞,治疗多达8次,RIT只针对癌细胞,而且只需注射一两次。
2002年9月,我注射了两剂最先进的RIT药物替伊莫单抗,之后病情逐渐减轻,身体基本健康。如果不是医疗创新,我的生活可能遭遇非常不一样的转折。
替伊莫单抗治疗方案中的关键部分是注入利妥昔单抗,该药可以减少血液中癌性B细胞数量。斯坦福大学(Stanford University)的研究人员利用美国国家卫生研究院(National Institutes of Health)的资助,在20世纪70年代和80年代发现该种B细胞技术。
但将想法变成切实可行的治疗方法需要大量时间和投资。如果不是当初研究人员离开斯坦福大学并于1985年成立Biotherapy Systems,进一步开发和商业化B细胞技术,医学发现可能永远没有机会变成在商业上可行的癌症疗法。
仅仅一年后,Biotherapy Systems与IDEC制药公司合并,成功实现了B细胞疗法。产品经过多年调整,IDEC于1993年开始利妥昔单抗临床试验。到1995年,生物技术巨头基因泰克(Genentech)与IDEC联手实施微调。
1997年,美国食品与药品管理局(FDA)终于批准,将利妥昔单抗的商标定为美罗华。
多亏1980年法律允许技术转让,否则该研究可能在斯坦福实验室就已经夭折。正因为《拜杜法》的推动,私营部门才成功开创了市场化药品。
我并不是唯一靠《拜杜法》支持的药物创新系统救回一命的病人。根据该法律,私营公司能够为病人提供数百种治疗方法,包括癫痫药物普瑞巴林、卵巢癌和乳腺癌药物紫杉醇,以及多发性硬化药物Tcelna等。
不过,目前社会活动团体正在向政客施压,要求利用法律中从未使用过的条款夺取新冠药物的专利权,这对私营制药公司和患者都不是好消息。该做法并无法律依据,因为《拜杜法》只允许政府在极少数情况下获得专利,比如当某家公司未广泛提供产品时。尽管面临各种压力,立法者仍需合作,维持《拜杜法》的保护力度。
因为事关人命。
患者应该感谢参议员拜赫和杜尔,因为两人认识到授权私营制药公司将政府资助的研究转化为药物和疗法无关党派。后来提案在国会通过,当时罗纳德•里根刚刚赢得大选,而吉米•卡特仍然在任。当年两党愿意携手推动公共卫生,帮助跟我一样与病魔抗争的人,现在这种精神应该延续。(财富中文网)
贝齐•德帕里是病人利益代言人,也是《癌症之地历险记》(Adventures in Cancer Land)一书作者。
译者:冯丰
审校:夏林
This Election Day, many Americans are wondering whether bipartisanship is even possible anymore.
For the millions suffering from cancer and other debilitating diseases, I hope so. Because 18 years ago, when I faced a deadly diagnosis of non-Hodgkin lymphoma (NHL), bipartisanship laid the foundation that gave me my life back.
The treatment that saved me resulted from years of research that would have amounted to nothing without the law authored by two senators, Indiana Democrat Birch Bayh and Kansas Republican Bob Dole, in 1980.
Known as the Bayh-Dole Act, this law allows universities, small businesses, and nonprofit organizations to own the early stage inventions they make in the course of their research using federal grants. These institutions can then license their intellectual property to private firms, which have the resources and experience to turn promising ideas into widely available medicines. Partnering with the private sector makes sense, because university laboratories usually lack the resources and manpower to nurture ideas through the lengthy and expensive research, testing, and development processes.
Prior to Bayh-Dole, the government retained ownership of intellectual property rights, and only occasionally translated them into real-world products for patient use. At the time the law passed, fewer than 5% of these government-owned inventions were licensed for commercial production. And not a single drug was developed from federally supported R&D when the government took patent rights away from the inventor.
Fortunately, Senators Bayh and Dole set partisanship aside to fix this logjam. Their landmark legislation has helped create a legal framework for private firms to pioneer more than 200 groundbreaking medical innovations—including the one that saved my life.
When I was diagnosed with an incurable form of NHL in January 2002, my only treatment option at the time was chemotherapy. It was known to slow the disease’s progression but it would inevitably return. Back then, the median life span from diagnosis to death was just eight years. My heart broke, knowing that wasn’t enough time to grow old with my husband or see my grandchildren through grade school.
But chemotherapy didn’t slow the progression of my disease. A few months into treatment—and in the nick of time—a new type of treatment for NHL hit the market: radioimmunotherapy (RIT). Unlike chemotherapy, which attacks both cancerous and healthy cells and requires up to eight treatments, RIT targets cancerous cells only, and takes only one or two injections.
In September 2002, I received two doses of the cutting-edge RIT drug Zevalin and have been in remission and healthy ever since. Without medical innovation, my life might have taken a very different turn.
A crucial part of Zevalin’s therapeutic regimen is the infusion of the drug rituximab, a medication designed to reduce the number of cancerous B cells in the blood. Using grants from the National Institutes of Health, researchers at Stanford University unearthed this B cell technology in the 1970s and 1980s.
But it takes a lot of time and investment to turn good ideas into tangible treatments. And this discovery may never have become a commercially viable cancer treatment had those researchers not left Stanford and formed Biotherapy Systems in 1985 to further develop and commercialize their B cell technology.
Just one year later, Biotherapy Systems merged with IDEC Pharmaceuticals to take its B cell therapy across the finish line. After years of tweaking its product, IDEC kicked off clinical trial testing of rituximab in 1993. And by 1995, biotech giant Genentech joined forces with IDEC to fine-tune the drug.
Finally, in 1997, the FDA approved their drug rituximab under the brand name Rituxan.
Without the technology transfer process enabled by the 1980 law, this research could have died in Stanford labs. But because of Bayh-Dole, the private sector has created a market-ready medicine.
I’m far from the only patient who owes her life to the drug innovation ecosystem Bayh-Dole supports. Under this law, private companies have been able to bring patients hundreds of treatments—including the epilepsy drug Lyrica, the ovarian and breast cancer therapy Taxol, and the multiple sclerosis medication Tcelna.
Now, though, activist groups are pressing politicians to exploit a never-used provision of the law to seize patent rights for COVID-19 medicine, to the detriment of private drug companies and patients. There would be no legal basis for this course of action—Bayh-Dole only allows the government to grab patents in rare instances such as where a company is not making a product widely available. Still, with the pressure on, our lawmakers need to cooperate to keep Bayh-Dole protections strong.
Lives literally depend on it.
Patients owe a debt of gratitude to senators Bayh and Dole, who recognized that empowering private drug companies to turn government-sponsored research into usable medicines and treatments is not a partisan issue. Their bill found its way through Congress at a divided moment, when Ronald Reagan had just won election but Jimmy Carter was still in office. Their willingness to work together in the service of public health and patients like me should inspire us today.
Betsy de Parry is a patient advocate and the author of Adventures in Cancer Land.






