辉瑞和BioNTech公司宣布的候选新冠病毒疫苗结果喜人,标志着他们在朝着战胜新冠疫情的道路上迈出了重要一步。在接下来的几个月中,即便做一次中等规模的疫苗分发,也能够保护数百万人免于疾病,挽救数万人的生命。
但如果要真正击退新冠肺炎,我们就需要群体免疫。只有一种方法可以确保这个目标的达成:为全球77亿人口中至少75%的人接种有效的疫苗。
要实现这一目标,我们必须对目前的生产、交付和疫苗获得人群的临时方法作出大幅调整。按照当前的计划,世界上四分之三的人口永远不可能得到疫苗接种——这意味着我们没有一个人会真正安全。
科研人员和许多国家的领导人拒绝通过感染的方式来达成群体免疫,因为这个方式增加了病毒在南北半球之间来回传播时产生季节性突变的恶性循环的风险——类似于流感的年际“进化”。
但这也并不是说,成功研发出有效的疫苗就意味着全部的答案。
据新冠肺炎疫苗实施计划(COVAX)称,各国政府应该优先向最易受病毒感染的人群,诸如卫生保健工作者、年长者和有潜在健康问题者等人群提供新冠疫苗。这样的举措将有效减少死亡人数,减轻卫生保健系统的压力。
但如果我们只给最易感的人群接种疫苗,那么新冠病毒将继续在世界上人口最多的一系列国家中,在常表现为无症状的年轻人群体中大面积蔓延。
今年9月,《科学》杂志(Science)发表了一篇关于印度年轻人感染率的研究,证明了接种疫苗计划的重要性。他们罹患新冠的比率比美国年轻人高得多,这意味着感染范围很广——因为印度的中位年龄是28岁,只有6%的人口被定义为老年人。但在美国,中位年龄是38岁,65岁及以上的人口占17%。
无症状感染也会产生后果。随着无症状感染的广泛传播,突变的可能性增加,新冠病毒成为永久性风险的可能性也会增加。新冠病毒的突变要比流感病毒慢得多,但每感染一个新的人,就更有可能产生突变。
如果我们未能及时为全球数十亿年轻人接种疫苗,任由他们感染,我们可能会在不经意间培育出一种新的流行病——因为一种突变的病毒可能会成为一种全新的疾病,对目前正在开发的疫苗无效,我们在群体免疫方面取得的任何进展也都将功亏一篑。
全球疫苗接种必须在短时间内完成,以确保病毒不会发生显著突变,逃离我们的掌控。我们将获得的终生免疫,不是来自某一种完美的疫苗,而是通过给我们中的大部分人接种疫苗,从而使病毒缺失宿主,逐渐消失。
疫苗研发和生产的努力让人动容,但由于致命缺陷——生产,它们距离通过接种来实现群体免疫差得还很远。
要理解这一挑战有多大,不妨以流感疫苗为例:每年流感疫苗的产量最高为15亿剂。从公开声明来看,III期临床试验的主要公司——Moderna、阿斯利康、强生和辉瑞及BioNTech——到2021年年底,这些公司加在一起只能为20亿人接种疫苗,还不到所需量的三分之一。
即便是这样的预测也已经相当乐观了。在目前临床试验的所有疫苗都获得批准的情况下,供应链方面的约束将束缚产量。制造商们将争夺关键成分有限的原料,包括核苷酸和酶等生物原料,以及瓶子和瓶盖这些更普通的配件。
一旦疫苗生产出来,交付过程也会面临一系列挑战。假设辉瑞、BioNTech的疫苗跨过了最后的监管障碍,其需要在零下80摄氏度的极端低温储存。对美国和其他能够负担得起每剂数千美元的国家来说,极低温冷链可能可行,但对墨西哥、巴西、尼日利亚、印度或印度尼西亚来说,可行性堪忧。在主要的疫苗竞争公司中,只有强生公司生产的一种疫苗在运输过程中不需要特殊处理。
为了克服冷链的挑战,我们需要能够在当地生产的疫苗,在最低的冷藏条件下实现交付,并在基本卫生保健基础设施下进行接种。要做到这一点,我们必须从更广泛的角度考虑疫苗生产和投资。
最初,大量投资都在美国和英国进行,现在,我们必须在世界各地投资那些技术足以制造疫苗,且成本低廉的公司。我们有能力通过信使RNA做到这一点——信使RNA将DNA转化成一种模拟冠状病毒上发现的蛋白质,帮助身体建立免疫。
一旦我们可以确保本地生产,创新性的交付解决方案就能够实现。我们可以把小冰箱装在可口可乐等送货卡车上,当这些卡车为偏远村庄的街角商店提供补给时,同时能够提供疫苗。教师和当地宗教领袖可以接受相关管理培训。
实现群体免疫的最后一公里困难重重,我们需要深思熟虑各种方法,充分利用世界各地的私营企业、卫生部门和非政府组织的智慧、技能和创造力。如果不能尽快这样做,所有这些痛苦和努力都将付诸东流。(财富中文网)
本文作者安德烈•扎鲁尔是总部位于波士顿的RNA研究、开发和制造公司GreenLight Biosciences的首席执行官。
编译:杨二一
辉瑞和BioNTech公司宣布的候选新冠病毒疫苗结果喜人,标志着他们在朝着战胜新冠疫情的道路上迈出了重要一步。在接下来的几个月中,即便做一次中等规模的疫苗分发,也能够保护数百万人免于疾病,挽救数万人的生命。
但如果要真正击退新冠肺炎,我们就需要群体免疫。只有一种方法可以确保这个目标的达成:为全球77亿人口中至少75%的人接种有效的疫苗。
要实现这一目标,我们必须对目前的生产、交付和疫苗获得人群的临时方法作出大幅调整。按照当前的计划,世界上四分之三的人口永远不可能得到疫苗接种——这意味着我们没有一个人会真正安全。
科研人员和许多国家的领导人拒绝通过感染的方式来达成群体免疫,因为这个方式增加了病毒在南北半球之间来回传播时产生季节性突变的恶性循环的风险——类似于流感的年际“进化”。
但这也并不是说,成功研发出有效的疫苗就意味着全部的答案。
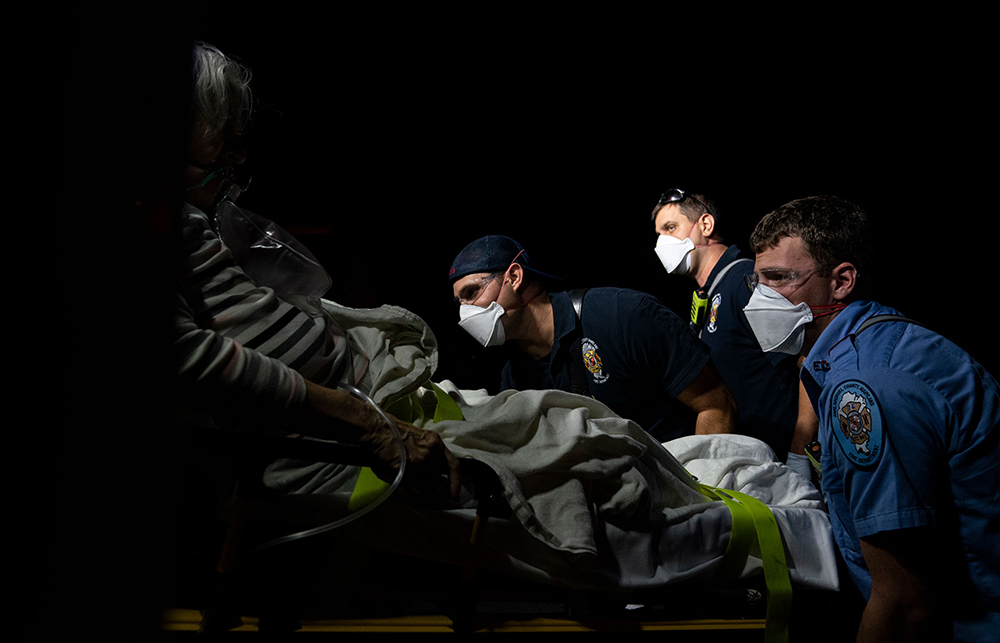
据新冠肺炎疫苗实施计划(COVAX)称,各国政府应该优先向最易受病毒感染的人群,诸如卫生保健工作者、年长者和有潜在健康问题者等人群提供新冠疫苗。这样的举措将有效减少死亡人数,减轻卫生保健系统的压力。
但如果我们只给最易感的人群接种疫苗,那么新冠病毒将继续在世界上人口最多的一系列国家中,在常表现为无症状的年轻人群体中大面积蔓延。
今年9月,《科学》杂志(Science)发表了一篇关于印度年轻人感染率的研究,证明了接种疫苗计划的重要性。他们罹患新冠的比率比美国年轻人高得多,这意味着感染范围很广——因为印度的中位年龄是28岁,只有6%的人口被定义为老年人。但在美国,中位年龄是38岁,65岁及以上的人口占17%。
无症状感染也会产生后果。随着无症状感染的广泛传播,突变的可能性增加,新冠病毒成为永久性风险的可能性也会增加。新冠病毒的突变要比流感病毒慢得多,但每感染一个新的人,就更有可能产生突变。
如果我们未能及时为全球数十亿年轻人接种疫苗,任由他们感染,我们可能会在不经意间培育出一种新的流行病——因为一种突变的病毒可能会成为一种全新的疾病,对目前正在开发的疫苗无效,我们在群体免疫方面取得的任何进展也都将功亏一篑。
全球疫苗接种必须在短时间内完成,以确保病毒不会发生显著突变,逃离我们的掌控。我们将获得的终生免疫,不是来自某一种完美的疫苗,而是通过给我们中的大部分人接种疫苗,从而使病毒缺失宿主,逐渐消失。
疫苗研发和生产的努力让人动容,但由于致命缺陷——生产,它们距离通过接种来实现群体免疫差得还很远。
要理解这一挑战有多大,不妨以流感疫苗为例:每年流感疫苗的产量最高为15亿剂。从公开声明来看,III期临床试验的主要公司——Moderna、阿斯利康、强生和辉瑞及BioNTech——到2021年年底,这些公司加在一起只能为20亿人接种疫苗,还不到所需量的三分之一。
即便是这样的预测也已经相当乐观了。在目前临床试验的所有疫苗都获得批准的情况下,供应链方面的约束将束缚产量。制造商们将争夺关键成分有限的原料,包括核苷酸和酶等生物原料,以及瓶子和瓶盖这些更普通的配件。
一旦疫苗生产出来,交付过程也会面临一系列挑战。假设辉瑞、BioNTech的疫苗跨过了最后的监管障碍,其需要在零下80摄氏度的极端低温储存。对美国和其他能够负担得起每剂数千美元的国家来说,极低温冷链可能可行,但对墨西哥、巴西、尼日利亚、印度或印度尼西亚来说,可行性堪忧。在主要的疫苗竞争公司中,只有强生公司生产的一种疫苗在运输过程中不需要特殊处理。
为了克服冷链的挑战,我们需要能够在当地生产的疫苗,在最低的冷藏条件下实现交付,并在基本卫生保健基础设施下进行接种。要做到这一点,我们必须从更广泛的角度考虑疫苗生产和投资。
最初,大量投资都在美国和英国进行,现在,我们必须在世界各地投资那些技术足以制造疫苗,且成本低廉的公司。我们有能力通过信使RNA做到这一点——信使RNA将DNA转化成一种模拟冠状病毒上发现的蛋白质,帮助身体建立免疫。
一旦我们可以确保本地生产,创新性的交付解决方案就能够实现。我们可以把小冰箱装在可口可乐等送货卡车上,当这些卡车为偏远村庄的街角商店提供补给时,同时能够提供疫苗。教师和当地宗教领袖可以接受相关管理培训。
实现群体免疫的最后一公里困难重重,我们需要深思熟虑各种方法,充分利用世界各地的私营企业、卫生部门和非政府组织的智慧、技能和创造力。如果不能尽快这样做,所有这些痛苦和努力都将付诸东流。(财富中文网)
本文作者安德烈•扎鲁尔是总部位于波士顿的RNA研究、开发和制造公司GreenLight Biosciences的首席执行官。
编译:杨二一
The promising results announced by Pfizer and BioNTech in their coronavirus vaccine candidate mark a significant step toward overcoming COVID-19. Even a modest deployment in the next few months could protect millions of people and save tens of thousands.
To beat back this pandemic, however, we need herd immunity. And there’s only one sure way to get that: We must inoculate at least 75% of the world’s 7.7 billion people with an effective vaccine.
Achieving this requires a sharp shift from our current ad hoc approach to production, delivery, and policies on who will get the vaccine. With the current plans, there is no way that three-quarters of the world will ever be vaccinated—which means none of us will truly be safe.
Reaching herd immunity via infection has been rejected by scientists and many world leaders because it raises the risk of creating a vicious cycle of seasonal mutation as the virus bounces between the world’s northern and southern hemispheres, similar to influenza’s annual evolution.
But that doesn’t mean that the discovery of a potent vaccine is the whole answer, either.
According to a new global partnership of health organizations called COVAX, authorities should prioritize giving a COVID vaccine to those most vulnerable to the virus—health care workers, the elderly, and those with underlying health conditions. This will reduce deaths and alleviate stress on health care systems.
Yet, if we vaccinate only the most vulnerable, the virus will continue to sweep through large swaths of often asymptomatic young people in some of the world’s most populous nations.
Evidence for the importance of a successful vaccination program came in September, when a study was published in Science about rates of infection in young people in India. They are getting COVID at a much higher rate than are young people in the U.S. That translates into widespread infection, because India’s median age is 28, with only 6% of the population defined as elderly. In the U.S., however, the median age is 38, and 17% of the population is 65 or older.
Infections without symptoms have consequences. With wide asymptomatic spread, there will be more mutations and more risk that the virus will become permanent. Coronaviruses mutate far more slowly than influenza viruses do, but the opportunity increases with each new person infected.
By failing to swiftly vaccinate the world’s billions of young people, and allowing them to become infected, we could inadvertently nurture a new pandemic. A mutated virus could become an entirely new disease that sidesteps the vaccines now under development and whatever progress we have made toward herd immunity.
Global vaccination must be done in a brief time frame to make sure the virus doesn’t significantly mutate and thus evade our grasp. We will all get lifetime immunity not by having a perfect vaccine, but by vaccinating so many of us that the virus has no hosts and fades away.
As impressive as vaccine development and production efforts have been to date, they will fall well short of achieving herd immunity through inoculation because of a shortcoming on the most basic level: production.
To understand the scale of the challenge, consider that production of the annual influenza vaccine tops out at 1.5 billion doses each year. From their public statements, it looks like the main companies in Phase III clinical trials—Moderna, AstraZeneca, Johnson & Johnson, and Pfizer/BioNTech—could together make only enough to inoculate 2 billion people by the end of 2021, less than a third of what is needed.
Even these projections are highly optimistic. In the unlikely event that all the vaccines currently in clinical trials are approved, supply chain constraints will hamper output. Manufacturers will be competing for the limited supply of critical components, including biological raw materials like nucleotides and enzymes as well as more mundane supplies such as vials and caps.
Once produced, delivery presents its own set of challenges. Pfizer/BioNTech’s vaccine, assuming that it passes the final regulatory hurdles, requires extreme-cold storage at minus 80 degrees Celsius. An extreme-cold chain may be feasible for the U.S. and other countries that can afford to pay thousands of dollars per dose, but this is not a viable solution for Mexico, Brazil, Nigeria, India, or Indonesia. Of the leading vaccine contenders, only the one from Johnson & Johnson doesn’t require special treatment during transportation.
To overcome this cold chain challenge, we need vaccines that can be manufactured locally, delivered with minimal refrigeration, and administered with basic health care infrastructure. And to do that, we have to think more broadly about vaccine production and investment.
The large initial investments were made in the U.S. and the U.K. Now we must invest in companies around the world that can use technology that can easily manufacture a virus—and cheaply. We have the capability to do that with messenger RNA, which translates DNA into proteins that mimic the proteins found on the coronavirus and help the body build immunity.
Once we can assure local production, we can figure out creative delivery solutions. We could put small refrigerators in Coca-Cola and other delivery trucks. As they resupply corner stores in remote villages, they could deliver vaccines. Teachers and religious leaders could be trained to administer it.
Getting down that last dusty mile to achieve vaccine-led herd immunity requires rethinking our approach and harnessing the combined intelligence, skills, and creativity of private companies, health authorities, and nongovernmental organizations around the world. Unless we do that, quickly, all this pain and effort will be wasted.
Andrey Zarur is CEO of GreenLight Biosciences, a Boston-based RNA research, development, and manufacturing company.






