今年7月份,世卫组织宣布猴痘为国际关注的突发公共卫生事件,这是世卫组织的最高级别预警。此时距第一例猴痘确诊病例在美国被发现仅仅过去了两个月。在世卫组织此次发布预警前,你可能从来都没有听说过猴痘这种病。但是现在,据美国疾控中心报告,美国各地已经出现了5000多例猴痘病例,而且全球至少已经确诊了1.8万例。
此时距新冠肺炎疫情爆发已经两年多了,全世界刚刚有了点重新开放的样子,很多人早已厌倦了戴口罩和保持社交距离等防疫措施。人们终于返回了阔别已久的学校、电影院和办公室,或多或少恢复了正常的生活。谁想到疫情却是一波未平,一波又起。很多人也根本没做好另一波疫情席卷全球的准备。
关于猴痘还有一种偏见,有人认为猴痘只会感染特定人群——总之不是像我这样的人。有些媒体还在不停拱火,利用了几十年来的种族主义偏见,硬把黑人跟猴子扯在一块儿,意思是黑人更容易感染猴痘。再加上目前猴痘疫情确实主要围绕同性恋群体传播,这就让不少人产生了一种虚假的安全感,并且助长了关于猴痘病毒的虚假信息,从而使很多人忽略了自己面临的风险。
如果说美国人能从新冠疫情刚爆发的那些日子里学到什么经验教训,那就是新冠病毒的感染者数量确实存在种族差异,但主要是因为白人采取的防范措施较少。纽约大学全球公共卫生学院流行病学教授丹妮尔·奥帕德医生指出,我们所有人都应该关注猴痘病毒。
那么关于猴痘,我们到底要掌握哪些防范常识呢?鉴于关于猴痘的谣言满天飞,着实唬住了不少人,下面我们就来辟个谣,为你解密关于猴痘那些事儿,包括它是如何感染的,我们应该如何预防猴痘,以及你离猴痘到底有多远。
谣言1:猴痘来自猴子
尽管名字叫猴痘,但猴痘并非来自于猴子。1958年,科学家在丹麦的一群科研用途的猴子身上首次发现了两起“痘状”病例。有记录的首例人感染猴痘病例是在1970年。
虽然猴子会得猴痘,但它们并不是猴痘的主要宿主。奥帕德医生指出,目前看来,猴痘病毒的主要宿主似乎是啮齿类动物。
猴痘与天花病毒应该属于同一家族,而且症状也与天花极为相似,只是更轻一些。其症状包括:
• 发烧
• 头痛
• 肌肉与背部疼痛
• 淋巴结肿大
• 恶寒
• 疲劳
• 喉咙痛、鼻塞、咳嗽
• 皮疹(可能出现在生殖器、肛门附近,或手、足、胸部等位置。)
据美国疾控中心称,猴痘的致命性是很低的。
谣言2:猴痘是一种性病
猴痘并非是一种性病。之所以会有这种误解,很可能是由于之前有报道称,男男性行为者易成为犯病高发群体。之前,世卫组织总干事谭德塞曾建议男同性恋者减少性伴侣数量,以减少猴痘的社区传播,这也是谭德塞唯一点名的一个群体,因此可能给部分人造成了猴痘只会通过性行为传播的错误印象。不过据专家称,事实并非如此。
奥帕德表示:“猴痘可以在人与人之间传播,所以如果我长了皮疹,而你长时间站在我身边,你的胳膊碰到了我胳膊上的皮疹,你就有感染的风险。”她还表示,人体的任何部位接触猴痘皮疹都有可能带来感染风险。“这也包括拥抱、亲吻和性行为。”
除了皮肤接触外,猴痘还可以通过呼吸道飞沫传染,并在怀孕期间由母亲传染给婴儿。你也可以通过接触被污染的物品(如床上用品、衣服、毛巾等)感染猴痘。目前,科学家仍在试图了解猴痘是否可以通过精液或阴道分泌物传染。
就如何避免感染猴痘,美国疾控中心给出了以下建议:
• 如果某人出现了猴痘样皮疹,则要避免与其进行皮肤接触(包括拥抱和性行为)。
• 避免与猴痘病人共用物品,或者接触其接触过的物品(如餐具等)。
• 经常用肥皂和消毒液洗手。
谣言3:猴痘只感染男男性行为者
“这绝对是谣言,”奥帕德医生表示:“不过是你还是我,是老人还是小孩,任何人都有可能感染猴痘,除非你以前得过。不光是男同性恋者会得猴痘,只不过是这次疫情的确诊病例里也有这一部分而已。”
“这种宣传方式给了人们一个抹黑同性恋群体的机会,这是一件不幸的事。”她补充道。
谣言4:我不需要担心得猴痘
奥帕德表示,我们也不必因为担心得猴痘,就到了惊慌失措闭门不出的地步。专家认为,不管是在人群密集场所还是在室内,只要大家都正常着装,那么你感染的风险还是比较低的,但也并非完全不会感染。专家还表示,我们从健身设施上或者从其他公共场所感染的可能性也是比较低的。目前看来,猴痘传播还是以密切接触者的传播为主。
“我们都应该保持关注,但没有必要惊慌失措。”奥帕德说。
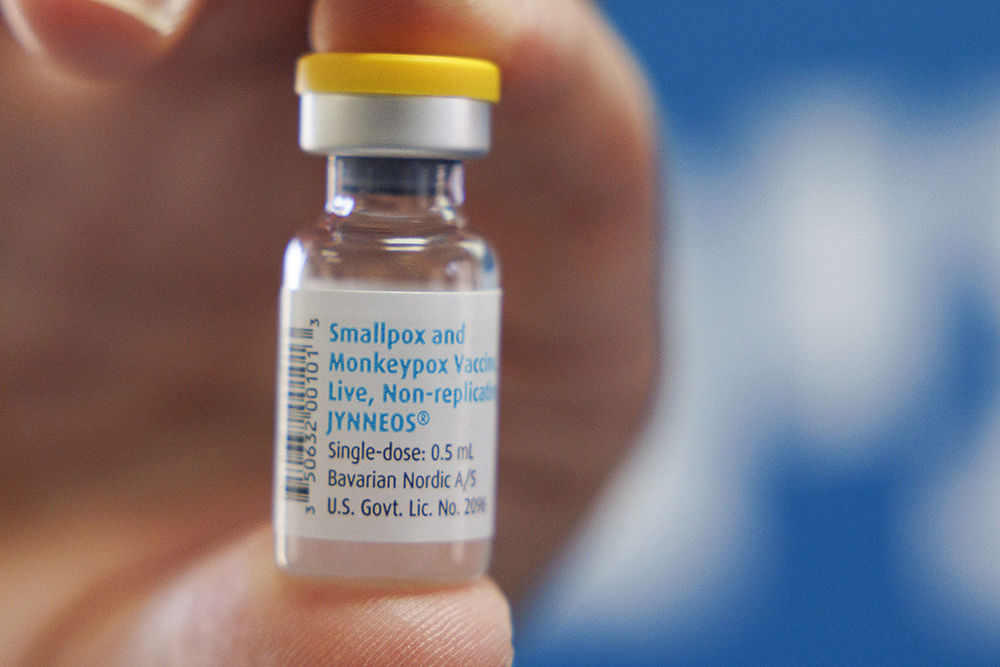
谣言5:所有人都可以打猴痘疫苗
并不是。美国现有两种天花疫苗可以用于预防猴痘,其中有一种供应量有限,但预计未来几个月内将有更多疫苗供应。美国疾控中心表示,任何有暴露风险的人,如果在3年内没有接种过天花疫苗,都应在暴露后的14天内接种疫苗,以减轻症状。这种接种策略又叫作环式免疫。
奥帕德表示:“一旦他们发现了一个确诊病例,就会划定密接人群,然后给他们接种疫苗。”其他人可能也适合接种猴痘疫苗,不过目前美国各州的接种政策不尽相同,但基本上仅限于那些有已知风险因素和暴露风险的人。
谣言6:药物无法治愈猴痘
有一款名叫TPOXX的抗病毒药物可以用于治疗猴痘,它以两周为一个疗程,目前处于供不应求的状态。
奥帕德表示,当前猴痘疫情的致死率很低,所以一般只采取支持性治疗,除非你有其他基础病或者有较高的死亡风险。
谣言7:猴痘很容易识别
人们很容易将猴痘误认为其他疾病,尤其夏天正是蚊虫叮咬高发的季节。奥帕德表示,猴痘的常见症状是全身性的皮疹或水痘,“但是也有人只长了几个疙瘩,不是每个人都有全身性的痘痕。”
奥帕德表示,最好的办法,就是在出现皮疹的第一时间就医检查。如果你认为自己可能已经接触了猴痘病毒,那么你应该立即自我隔离,避免接触他人,并且立即就诊。(财富中文网)
译者:朴成奎
今年7月份,世卫组织宣布猴痘为国际关注的突发公共卫生事件,这是世卫组织的最高级别预警。此时距第一例猴痘确诊病例在美国被发现仅仅过去了两个月。在世卫组织此次发布预警前,你可能从来都没有听说过猴痘这种病。但是现在,据美国疾控中心报告,美国各地已经出现了5000多例猴痘病例,而且全球至少已经确诊了1.8万例。
此时距新冠肺炎疫情爆发已经两年多了,全世界刚刚有了点重新开放的样子,很多人早已厌倦了戴口罩和保持社交距离等防疫措施。人们终于返回了阔别已久的学校、电影院和办公室,或多或少恢复了正常的生活。谁想到疫情却是一波未平,一波又起。很多人也根本没做好另一波疫情席卷全球的准备。
关于猴痘还有一种偏见,有人认为猴痘只会感染特定人群——总之不是像我这样的人。有些媒体还在不停拱火,利用了几十年来的种族主义偏见,硬把黑人跟猴子扯在一块儿,意思是黑人更容易感染猴痘。再加上目前猴痘疫情确实主要围绕同性恋群体传播,这就让不少人产生了一种虚假的安全感,并且助长了关于猴痘病毒的虚假信息,从而使很多人忽略了自己面临的风险。
如果说美国人能从新冠疫情刚爆发的那些日子里学到什么经验教训,那就是新冠病毒的感染者数量确实存在种族差异,但主要是因为白人采取的防范措施较少。纽约大学全球公共卫生学院流行病学教授丹妮尔·奥帕德医生指出,我们所有人都应该关注猴痘病毒。
那么关于猴痘,我们到底要掌握哪些防范常识呢?鉴于关于猴痘的谣言满天飞,着实唬住了不少人,下面我们就来辟个谣,为你解密关于猴痘那些事儿,包括它是如何感染的,我们应该如何预防猴痘,以及你离猴痘到底有多远。
谣言1:猴痘来自猴子
尽管名字叫猴痘,但猴痘并非来自于猴子。1958年,科学家在丹麦的一群科研用途的猴子身上首次发现了两起“痘状”病例。有记录的首例人感染猴痘病例是在1970年。
虽然猴子会得猴痘,但它们并不是猴痘的主要宿主。奥帕德医生指出,目前看来,猴痘病毒的主要宿主似乎是啮齿类动物。
猴痘与天花病毒应该属于同一家族,而且症状也与天花极为相似,只是更轻一些。其症状包括:
• 发烧
• 头痛
• 肌肉与背部疼痛
• 淋巴结肿大
• 恶寒
• 疲劳
• 喉咙痛、鼻塞、咳嗽
• 皮疹(可能出现在生殖器、肛门附近,或手、足、胸部等位置。)
据美国疾控中心称,猴痘的致命性是很低的。
谣言2:猴痘是一种性病
猴痘并非是一种性病。之所以会有这种误解,很可能是由于之前有报道称,男男性行为者易成为犯病高发群体。之前,世卫组织总干事谭德塞曾建议男同性恋者减少性伴侣数量,以减少猴痘的社区传播,这也是谭德塞唯一点名的一个群体,因此可能给部分人造成了猴痘只会通过性行为传播的错误印象。不过据专家称,事实并非如此。
奥帕德表示:“猴痘可以在人与人之间传播,所以如果我长了皮疹,而你长时间站在我身边,你的胳膊碰到了我胳膊上的皮疹,你就有感染的风险。”她还表示,人体的任何部位接触猴痘皮疹都有可能带来感染风险。“这也包括拥抱、亲吻和性行为。”
除了皮肤接触外,猴痘还可以通过呼吸道飞沫传染,并在怀孕期间由母亲传染给婴儿。你也可以通过接触被污染的物品(如床上用品、衣服、毛巾等)感染猴痘。目前,科学家仍在试图了解猴痘是否可以通过精液或阴道分泌物传染。
就如何避免感染猴痘,美国疾控中心给出了以下建议:
• 如果某人出现了猴痘样皮疹,则要避免与其进行皮肤接触(包括拥抱和性行为)。
• 避免与猴痘病人共用物品,或者接触其接触过的物品(如餐具等)。
• 经常用肥皂和消毒液洗手。
谣言3:猴痘只感染男男性行为者
“这绝对是谣言,”奥帕德医生表示:“不过是你还是我,是老人还是小孩,任何人都有可能感染猴痘,除非你以前得过。不光是男同性恋者会得猴痘,只不过是这次疫情的确诊病例里也有这一部分而已。”
“这种宣传方式给了人们一个抹黑同性恋群体的机会,这是一件不幸的事。”她补充道。
谣言4:我不需要担心得猴痘
奥帕德表示,我们也不必因为担心得猴痘,就到了惊慌失措闭门不出的地步。专家认为,不管是在人群密集场所还是在室内,只要大家都正常着装,那么你感染的风险还是比较低的,但也并非完全不会感染。专家还表示,我们从健身设施上或者从其他公共场所感染的可能性也是比较低的。目前看来,猴痘传播还是以密切接触者的传播为主。
“我们都应该保持关注,但没有必要惊慌失措。”奥帕德说。
谣言5:所有人都可以打猴痘疫苗
并不是。美国现有两种天花疫苗可以用于预防猴痘,其中有一种供应量有限,但预计未来几个月内将有更多疫苗供应。美国疾控中心表示,任何有暴露风险的人,如果在3年内没有接种过天花疫苗,都应在暴露后的14天内接种疫苗,以减轻症状。这种接种策略又叫作环式免疫。
奥帕德表示:“一旦他们发现了一个确诊病例,就会划定密接人群,然后给他们接种疫苗。”其他人可能也适合接种猴痘疫苗,不过目前美国各州的接种政策不尽相同,但基本上仅限于那些有已知风险因素和暴露风险的人。
谣言6:药物无法治愈猴痘
有一款名叫TPOXX的抗病毒药物可以用于治疗猴痘,它以两周为一个疗程,目前处于供不应求的状态。
奥帕德表示,当前猴痘疫情的致死率很低,所以一般只采取支持性治疗,除非你有其他基础病或者有较高的死亡风险。
谣言7:猴痘很容易识别
人们很容易将猴痘误认为其他疾病,尤其夏天正是蚊虫叮咬高发的季节。奥帕德表示,猴痘的常见症状是全身性的皮疹或水痘,“但是也有人只长了几个疙瘩,不是每个人都有全身性的痘痕。”
奥帕德表示,最好的办法,就是在出现皮疹的第一时间就医检查。如果你认为自己可能已经接触了猴痘病毒,那么你应该立即自我隔离,避免接触他人,并且立即就诊。(财富中文网)
译者:朴成奎
You may not have heard of monkeypox until the World Health Organization declared it a global public health emergency of international concern—its highest alert level—in July, just two months after the first case in the current outbreak was identified in the U.S. Now, the Centers for Disease Control and Prevention is reporting more than 5,000 cases of monkeypox across the country, though there are at least 18,000 worldwide.
The monkeypox outbreak comes more than two years into the COVID-19 pandemic, as the world has reopened and many people have grown weary of taking preventive measures, like wearing masks and social distancing. We’ve returned to schools, to movies, to the office, to normal-ish, and so many of us have not engaged with the constantly evolving news about yet another viral disease sweeping the globe.
And then there is bias—the idea that monkeypox only affects certain people. People who aren’t like you. In fact, some media outlets came under fire recently for using decades-old images of Black people in their reporting on monkeypox, playing into stereotypes around their criminality and racist tropes that associate Black people with monkeys. This coupled with the fact that the current outbreak is circulating among the LGBTQ community, has given some people a false sense of security, and fueled, not only misinformation about how monkeypox is spread, but who’s at risk.
If we learned anything from the early days of the COVID crisis, it’s that when racial disparities in who contracted COVID-19 were highlighted, white people took fewer precautions. But we should all be concerned about monkeypox, says Dr. Danielle Ompad, professor of epidemiology at New York University School of Global Public Health.
Whether you’re confused by the headlines or exhausted trying to make sense of them, you’re not alone. Here, an epidemiologist cuts through the swirl of misinformation to help you understand the facts about monkeypox, including how it’s contracted, prevented, and how worried you should really be.
Myth 1: Monkey pox comes from monkeys.
Despite its name, monkeypox does not come from monkeys. The disease earned the name when two “pox-like” outbreaks happened among colonies of research monkeys in 1958 in Denmark. The first human case of monkeypox was documented in 1970.
While monkeys can get monkeypox, they are not the reservoir (where a disease typically grows and multiplies). The reservoir seems to be rodents, says Ompad.
Monkeypox is part of the same family of viruses that causes smallpox and has similar, but milder, symptoms, which include:
• Fever
• Headache
• muscle aches and backache
• swollen lymph nodes
• Chills
• Fatigue
• sore throat, nasal congestion, cough
• a rash that may be on or near the genitals or anus, but could also be on other areas like the feet, hands, and chest.
Monkeypox is rarely fatal, according to the CDC.
Myth 2: Monkeypox is a sexually transmitted infection (STI)
It’s not. But this point of confusion is likely because the strongest warnings about the spread of monkeypox have been aimed at men who have sex with men. They are also the only group that WHO director general Dr. Tedros Adhanom Ghebreyesus advised to limit their sex partners to reduce community spread, which has given the false impression that the disease is spread only through sexual contact. Experts caution that’s not true.
“Monkeypox can be transmitted person to person, so that means if I have a rash, and you’re standing next to me with prolonged contact and your arm touches the rash on my arm, you’re at risk for transmission,” says Ompad. Any close contact with a rash puts you at risk “so that includes hugging, kissing, and sex as well,” she says.
In addition to skin-to-skin contact, monkeypox can also be passed by respiratory droplets and from mother to child during pregnancy. You can be also be infected with monkeypox through contact with contaminated items like bedding, clothes, and towels.
Scientists are still trying to understand if monkeypox can be spread through semen or vaginal fluids.
To help prevent monkeypox, the CDC recommends:
• Avoid skin-to-skin contact (including hugging, cuddling, or having sex) with anyone who has a rash that looks like monkeypox.
• Avoid sharing or touching objects a person with monkeypox has used, including utensils.
• Wash your hands with soap and water or use hand sanitizer frequently.
Myth 3: Monkeypox only affects men who have sex with men.
“That’s absolutely not true,” says Ompad. “It can affect anybody, except maybe if you’ve had a previous infection. I can get it, you can get it, children can get it, and grandmas can get it. It’s not only gay men who are at risk for getting this disease, that’s just where the clusters are in this particular outbreak,” she says.
“The way the messaging has played out has given people an opportunity to say negative things about the LGBTQ community. It’s really unfortunate,” she adds.
Myth 4: I shouldn’t worry about monkeypox.
We shouldn’t be worried to the point where we’re panicking and staying inside all the time, Ompad says. Experts say your risk is relatively low, but not zero, in crowds and indoor public places where people are fully clothed. They also say that you’re not likely to contract it from gym equipment or other surfaces in public spaces. Right now, transmission is the result of close, intimate contact.
“We should all be paying attention, but we shouldn’t be freaked out,” Ompad says.
Myth 5: Anyone can get a monkeypox vaccine.
Not really. In the U.S., there are two types of smallpox vaccine used to prevent monkeypox, and one of them is in limited supply, though more is expected to be available in the coming months. The CDC says anyone exposed to monkeypox who hasn’t had a smallpox vaccine within three years, should get vaccinated for monkeypox within four and and no more than 14 days of exposure, in order to reduce symptoms. This is a strategy called ring vaccination.
“Once they identify a case, they identify their close contacts and give them the vaccination,” Ompad says. Others may be eligible for monkeypox vaccination, but it really varies by state and generally limited to those with known risk factors and people who have been exposed.
Myth 6: Monkeypox can’t be treated with medication.
There is one approved medication for monkeypox, a two-week course of an antiviral drug called TPOXX, and it is in short supply.
The mortality rate for the current outbreak is low, notes Ompad, so the typical treatment is just supportive care, unless you have a preexisting condition or are at high risk of death.
Myth 7: Monkeypox is easy to recognize.
It can be quite easy to mistake monkeypox for something else, especially in bug bite season. Ompad points out that while a common symptom is a rash or sores across the body, “monkeypox can also be just a few spots; not everyone will have fully disseminated pox marks,” she says.
The best thing to do is get checked out the minute you develop a rash, says Ompad. And if you think you might have been exposed to monkeypox, isolate, and stay away from other people until you can talk to your doctor.






